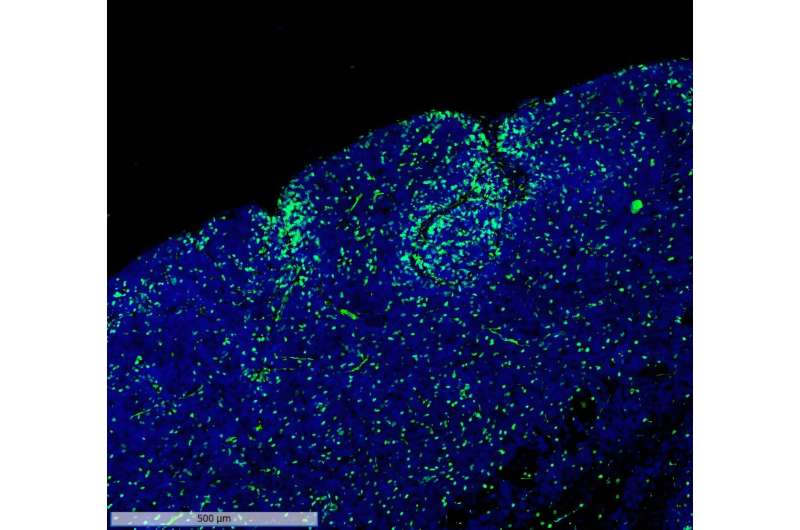
Recent research has unveiled a promising new therapy for treating childhood brain cancer, specifically targeting a type of tumor known as glioma. Scientists have identified a novel approach that involves using a combination of existing medications to enhance treatment effectiveness. This innovative therapy works by targeting specific genetic mutations commonly found in these tumors, allowing for a more personalized treatment plan tailored to the individual child’s cancer profile. The early results from clinical trials have been encouraging, suggesting that this targeted approach could significantly improve survival rates and reduce the side effects typically associated with conventional treatments.
Furthermore, the research emphasizes the importance of collaboration between pediatric oncologists and geneticists to develop more effective treatment strategies. As scientists continue to uncover the complex genetic landscape of childhood brain tumors, this therapy highlights the potential of precision medicine in oncology. By focusing on the unique genetic makeup of each tumor, this new treatment not only holds the promise of better outcomes for young patients but also paves the way for future advancements in the fight against pediatric cancers. Continued research and clinical trials will be essential in validating these findings and bringing this groundbreaking therapy to children in need. Click for More Details